Medical VR’s long history
Applications of virtual reality (VR) and augmented reality (AR) have been around since at least the early 1990s. Numerous early applications, including a VR-based surgical planning process using hardware developed by NASA, often had to do with helping doctors visualize complex anatomy with the aim of facilitating surgical planning and training.
We’re all now aware of the recent emergence of modern VR and AR iterations, facilitated by a succession of technological breakthroughs in tracking systems, small displays, and computing capability. The medical community is quickly adopting this new transformative tech. With over 12,000 publications using common search terms for VR/AR applications in healthcare and a projected global healthcare market of $5.1 billion by 2025, it’s worth it to better understand the roles these technology can play in the medical field.
Breaking down the roles
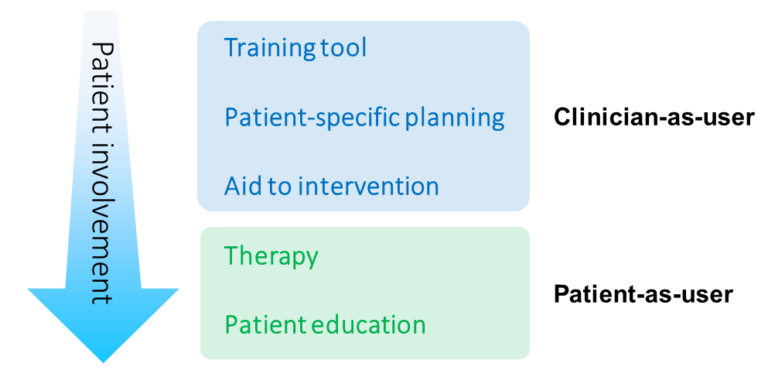
Modern healthcare applications include medical education, surgical planning, facilitating communications, therapeutic interventions, and more. With such a diverse set of applications under the umbrella of healthcare or medicine, it’s useful to categorize the different uses to better understand what people mean when they say “VR/AR in healthcare.”
Luckily there’s a single variable that does a good job of teasing out the different roles for VR and how those roles are distinct. That variable is how involved the patient is in the given process under consideration; their proximity in the process to a given intervention.
VR as a clinician education and training tool
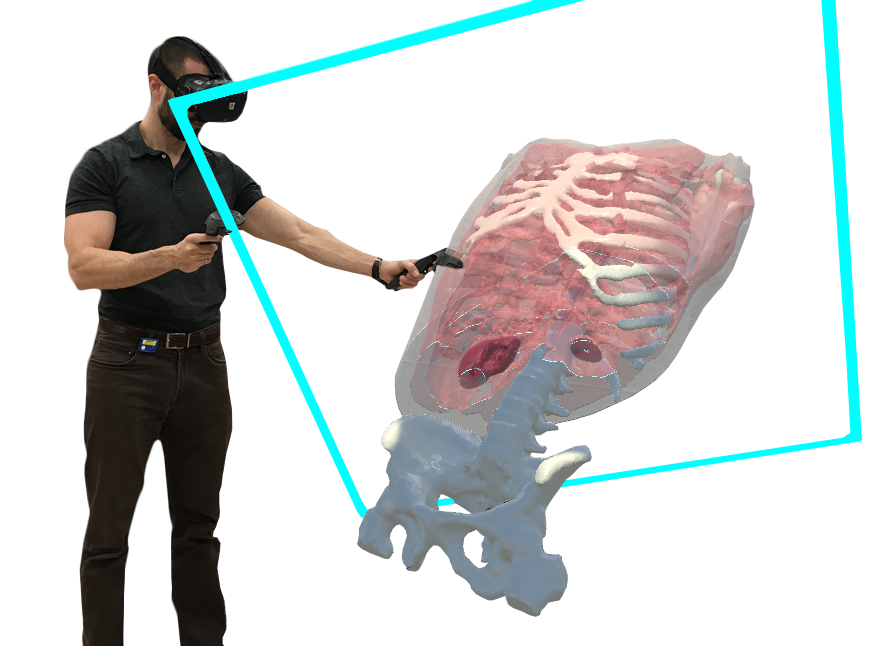
The role for VR/AR in healthcare with the least direct patient involvement is in educating and training healthcare professionals. Almost universally, the first time we show our product to someone new, they suggest that it would be great for teaching or learning anatomy. This is because learning human anatomy can be a difficult task: using 2D form factors (like images and textbooks) to form a 3D cognitive model of the body is challenging. The value that mixed reality technologies like VR and AR bring to this task is obvious and so it’s no surprise that several human anatomy education applications already exist like 3D Organon VR, ShareCare, Visible Body, and Complete Anatomy. Beyond learning the human body, immersive experiences can also be used for things like helping healthcare professionals understand what it’s like to be a patient.
As physicians begin to specialize, VR can be used for more targeted education such as simulations for surgical training. A particularly creative company called Enduvo has even created a VR-based education platform, where users can create their own immersive lessons using 3D models, environments and recorded 3D lectures.
Patient-specific planning
If we now consider situations that involve specific patient cases, then the next category emerges as patient-specific planning. Here virtual and augmented reality join more established novel technologies such as 3D printing which has already been driving planning improvements in surgery due to content creation efforts in radiology.
By viewing 3D models that radiologists derive from medical images or by interacting with 3D renderings of un-segmented images (using volume rendering), healthcare professionals can gain a better understanding of difficult cases and plan the course of their interventions more accurately.
Due to these technologies, patient-specific planning is changing rapidly which is why we’re using VR itself to better meet the growing demand for individualized 3D content and models.
Intervention aid
With patient-specific models or other useful guidance in hand, the patient comes into immediate proximity. The potential to aid interventions is where augmented reality shines while virtual reality – immersing the user in an environment that shuts out the real world – has little use. Giving surgeons on-demand X-Ray vision and providing fluidly displayed information overlays is the holy grail of mixed reality technology, and while current implementations provide a great deal of value, in our opinion, the true winner in this application will be revealed by future technological iterations.
That said, current AR-based surgical intervention aids are beginning to achieve FDA clearance. And in future years, when augmented reality applications live within pervasive app-based smartphone-like platforms, one can easily imagine how a great number of clinical tasks beyond surgery will be significant facilitated by integrated, 3D, and world-cognizant information.
Clinician-as-user and patient-as-user
VR as a therapeutic intervention
If you’ve experienced networked VR applications, you’ll know that there’s a surprisingly engaging quality to interacting with someone’s 3D avatar in a fully simulated world. It’s no surprise, then, that researchers are already looking at using VR to facilitate telemedicine.
VR/AR for patient education

Summary
By knowing how to categorize and understand all the roles that this technology can play in healthcare and medicine, we can start looking at the field with a keen eye for potential improvements. Afterall, when creative worlds of one’s imagining are at one’s disposal, there’s a lot of opportunity to explore. The first step in better understanding how VR and AR can be applied to medicine is made by creating a distinction between clinician-as-user and patient-as-user applications. Within those two categories, we can also further stratify applications by how closely they require direct patient involvement. This ranges from general clinical education all the way to aiding physicians in their actual patient-specific interventions on the clinician-as-user side of things and distinguishes between doctor-led therapeutic interventions and more self-guided educational applications on the patient-as-user side.
– Justin Sutherland
