Surgical planning is a critical aspect of medical practice, determining the success of procedures and the safety of patients. Over the years, technological advancements have transformed the way surgeons approach planning. We are now entering an era where spatial computing and mixed reality technologies provide a complete picture of the surgical landscape. To best understand this transformation, it’s instructive to look back at two previous eras of surgical planning: the pre-3D imaging era and the 3D imaging with 2D visualization era.
Era 1: The Pre-3D Imaging Era (Before Late 1970s)
Before the late 1970s, surgeons lacked access to 3D medical images like CT scans and MRIs. Surgical planning relied heavily on physical examinations, basic 2D X-rays, and the accumulated experience of the surgeons.
Challenges
The absence of detailed imaging left surgeons with limited information, leading to higher uncertainty and risk during procedures. Exploratory surgeries were often necessary to understand the internal structures, which increased the risk for patients. Surgeons faced a high cognitive load, needing to mentally reconstruct anatomical structures from minimal data, often resulting in incomplete and inaccurate understandings of the patient’s anatomy.
Era 2: The 3D Imaging with 2D Visualization Era

The advent of 3D imaging technologies like CT and MRI scans marked a significant leap forward. These technologies provided detailed, cross-sectional views of the human body, revolutionizing surgical planning.
With these advancements, surgeons could visualize complex anatomical structures with greater detail and accuracy. Planning became more precise, leading to better outcomes compared to the pre-3D era. However, this era still had its limitations: planning was still done with an incomplete picture.
Challenges
Interactions with 3D images were still conducted through 2D screens, abstracting the true spatial relationships of anatomical structures. This led to residual uncertainties due to limited depth perception and spatial awareness. Surgeons had to exert significant cognitive effort to interpret and mentally reconstruct 3D information from 2D slices. Misinterpretations and oversights were common, as critical anatomical details could be easily missed, and many decisions about surgical plans are still left to be made during the procedures themselves.
Era 3: The Era of Spatial Computing and Mixed Reality
Overview
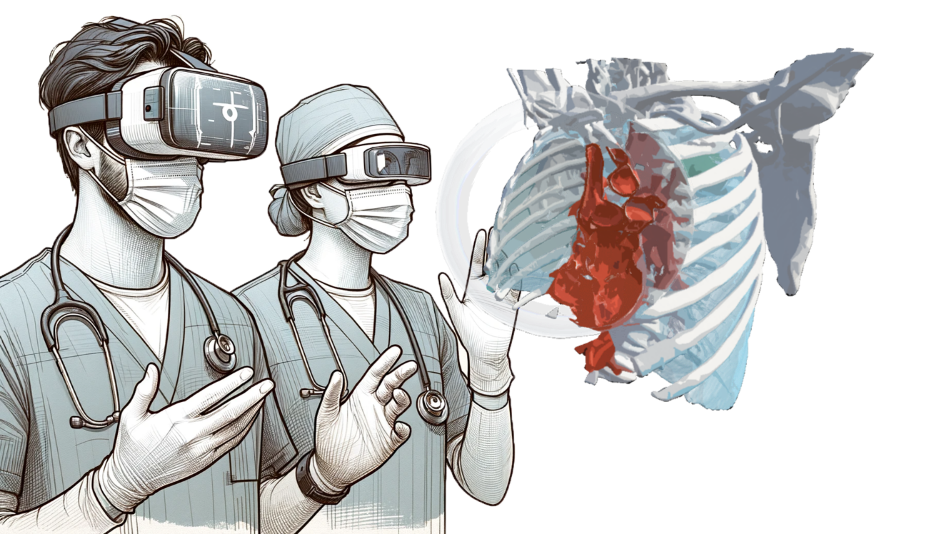
We are now entering the era of spatial computing and mixed reality, where technologies like VR and AR offer immersive 3D visualization and interaction with medical images – providing a more complete picture. This era promises to revolutionize surgical planning by providing a more complete and intuitive understanding of patient anatomy.
Advantages
Spatial computing allows surgeons to immerse themselves in a 3D environment, interacting with medical images in ways that were previously impossible. This enhances depth perception and spatial awareness, significantly reducing the cognitive load. Surgeons can now intuitively understand complex anatomical relationships, making planning more accurate and efficient.
Evidence of Benefits
A growing body of evidence supports the benefits of VR planning in surgery:
- Reduced operative times1,7,8,9,11
- Studies have shown that VR planning can lead to shorter surgical procedures
- Reduced blood loss1,6,8
- VR visualization helps in more precise planning, reducing intraoperative blood loss.
- Shorter hospital stays1,8
- Patients benefit from quicker recoveries and shorter hospital stays.
- Fewer fluoroscopic images1,6,11
- VR planning reduces the need for intraoperative imaging, minimizing radiation exposure to patients and providers.
- Improved assessment of cases2,6,10
- Surgeons can better assess and plan for complex cases.
- Improved clinical outcomes3,4,7
- Overall, patients experience better clinical outcomes due to more precise and effective surgical planning.
- Alteration of surgical plans5,6
- The user of VR frequently leads to alteration of surgical plans based on better understanding of patient anatomy and 3D relationships.
Future Prospects
As spatial computing technology continues to evolve, its integration into surgical education and training will further enhance its impact. Ongoing research and development will likely expand the capabilities and applications of mixed reality in healthcare, offering even more sophisticated tools for surgeons.
Conclusion
The era of spatial computing is transforming surgical planning by providing a complete picture that was previously unattainable. By overcoming the limitations of past eras and leveraging the immersive power of VR and mixed reality, we are poised to see significant advancements in surgical outcomes and patient care. The journey from no access to 3D images, to interacting with 3D images on 2D screens, to the immersive world of spatial computing, highlights the continuous evolution and improvement in surgical planning. As we embrace this new era, the possibilities for innovation and improvement in medical practice are boundless.
- Chen S, et al (2020) Evaluation of the computer-assisted virtual surgical technology in preoperative planning for distal femoral fracture. Injury 51(2):443–451
- Kenngott HG, et al (2022) IMHOTEP: cross-professional evaluation of a three-dimensional virtual reality system for interactive surgical operation planning…for complex liver surgery…. Surg Endosc 36(1):126–134
- Kockro RA, et al (2016) Aneurysm surgery with preoperative three-dimensional planning in a virtual reality environment: technique and outcome analysis. World Neurosurg 96:489–499
- Louis RG, et al (2021) Early experience with virtual and synchronized augmented reality platform for preoperative planning and intraoperative navigation: a case series. Oper Neurosurg (Hagerstown) 21(4):189–196
- McDonald M, Shirk DJ (2021) Application of three-dimensional virtual reality models to improve the pre-surgical plan for robotic partial nephrectomy. JSLS 25(3):e2021.00011
- Parkhomenko E, et al (2019) Pilot assessment of immersive virtual reality renal models as an educational and preoperative planning tool for percutaneous nephrolithotomy. J Endourol 33(4):283–288
- Shakya S, et al (2022) Virtual surgical planning is a useful tool in the surgical management of mandibular condylar fractures. Chin J Traumatol 25(3):151–155
- Shirk JD, et al (2019) Effect of 3-dimensional virtual reality models for surgical planning of robotic-assisted partial nephrectomy on surgical outcomes: a randomized clinical trial. JAMA Netw Open 2(9):e1911598
- Steineke TC, Barbery D (2021) Microsurgical clipping of middle cerebral artery aneurysms: preoperative planning using virtual reality to reduce procedure time. Neurosurg Focus 51(2):E12
- Sugiyama T, et al (2021) Immersive 3-dimensional virtual reality modeling for case-specific presurgical discussions in cerebrovascular neurosurgery. Oper Neurosurg (Hagerstown) 20(3):289–299
- Zheng C, et al (2019) Development of a virtual reality preoperative planning system for postlateral endoscopic lumbar discectomy surgery and its clinical application. World Neurosurg 123:e1–e8
